Cardiac Surgery
Why do you need bypass surgery?
Patients with a narrowing or blockage in the coronary arteries diagnosed by a coronary angiogram may be considered for coronary artery bypass grafting (CABG). As the techniques and technology of angioplasty and stent procedures have improved the numbers of patients undergoing CABG has fallen significantly. In some patients, however, CABG remains clearly the best treatment with the best long term outcome.
All patients who are referred for CABG to a cardiac surgeon are first seen and assessed by a cardiologist or heart specialist who determines the treatment options, often in discussion with a team of other cardiologists and cardiac surgeons.
What happens during bypass surgery?
CABG is a major operation that usually lasts between two and six hours. Pre-operative medications are often administered by mouth, muscular or subcutaneous injection, or intravenously. Patients receive general anaesthetic and are completely asleep.
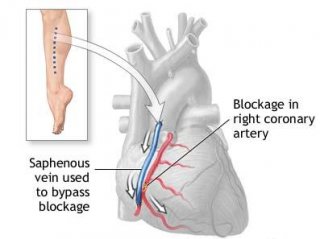
During CABG the chest bone is separated, and the ribs are spread apart to allow visible and physical access to the heart. In most instances, blood circulation and breathing functions will be taken over by a heart-lung machine, although in some cases CABG can be performed on a beating heart. The cardiac surgeon uses a piece of vein or artery to form a bypass to enable blood to go around the blockage. Several blockages can be bypassed during surgery.
What is a graft?
A graft is a blood vessel that has been created to bypass a blocked artery. It is usually taken from the internal mammary artery in the chest, the saphenous veins from the leg, or in sometimes from the radial artery in the arm. The graft is attached above and below the area in the artery where there is a blockage, so that the blood can use the new, unblocked path to flow freely to the heart muscle.
From stress tests, angiograms and intravascular ultrasounds the cardiologist is able to determine exactly how much of the heart structure needs repair. Some patients undergo double, triple or even quadruple bypasses, based on their specific needs. The number of grafts is not as important as the bypass of the necessary blockages.
CABG is most successful when the blockages are discrete in the large part of the arteries before the arteries have branched. In contrast CABG is technically challenging with lower success rates in smaller vessels or where there is diffuse narrowing. The pattern of artery narrowing is be determined by the coronary angiogram.
Will my heart be stopped?
In most cases the blood circulation and breathing functions are taken over totally by a heart-lung machine during surgery, also known as cardiopulmonary bypass. However, some CABG surgery is being performed while the heart is still beating (called the off-pump technique). The beating heart approach may reduce the risk of brain injury, stroke and other complications associated with the heart-lung machine, and leads to a shorter hospital stay for patients.
Are there any transfusions involved? Should I bank my own blood?
Ordinarily, as with any serious heart surgery, blood transfusions are necessary during bypass surgery. The blood used for your surgery will be matched by type and Rh factor, and provided by a local blood bank. Unless the surgery is scheduled in less than 72 hours, and if the doctor gives the patient permission, arrangements can be made for banking the patient’s own blood for surgery.
What are the risks?
The current success rate for bypass surgery is 95 to 98 percent, meaning that between 2 and 5 percent of all patients have complications, including death. The survival rate has improved over time, but depends on the patient’s overall condition including any lung disease, other artery disease, previous strokes and kidney function.
As with any surgical procedure, there are risks of infection and heavy bleeding. There also are risks associated with anesthesia. These can include adverse reactions to medication and breathing problems. Postoperative pneumonia and wound infection also are common complications arising from open-heart surgery.
How successful is bypass surgery? Can I expect to live a long life?
Studies have shown in 80 to 95 percent of patients, bypasses made with segments of the mammary artery still performed efficiently 10 years after surgery. Two-thirds to 75 percent of patients who received grafts from leg veins still had satisfactorily unrestricted blood flow after 10 years.
Remember that even if your graft becomes blocked, you may not need additional bypass surgery. However, you may be a candidate for balloon angioplasty and insertion of a stent.
Where will the surgery take place, and how can I prepare for it?
The surgery will be performed in a hospital operating room.
Some individuals are unaware of the extent to which their arteries are clogged until they have a heart attack. In cases such as these, a cardiologist or emergency room doctor will probably quickly determine whether bypass surgery can be successful. There might be little time to discuss options or extensively educate you or your family.
Ideally, you have discussed your health history with a cardiologist. You may have been treated with cholesterol lowering or blood pressure-lowering medications for some time. However, because of chest pain or test results from a stress test, it is evident to your doctor that bypass surgery is a necessary step. If you need additional input from your doctor, or perhaps a second opinion, it is in your best interest to get it as quickly as possible. In most cases, advanced coronary artery disease should be treated as soon as possible, to avoid further damage to the heart.
How long is the surgery?
Typically, traditional bypass surgery takes between two and six hours, depending on the number of bypasses to be performed. Minimally invasive bypass surgery usually takes two to three hours.
Further information on cardiac surgery, recovery and returning to normal activity will be provided by the cardiac surgical team based on the local policy and protocols.